ABOUT HITECK
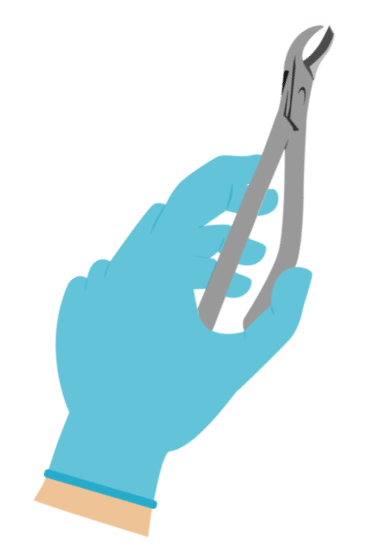
OUR SERVICES
PRODUCT SOURCING & CONSULTATION

NEW PRODUCT DESIGN

PROPER REPROCESSING TECHNIQUES

INFECTION CONTROL GUIDANCE

where it all started
birth
Started OEM manufacturing medical devices for international brands. Only a handful of SKU's in production.

Germany
After 11 years of manufacturinhg OEM instruments, we opened up our local branch in heart of Tuttlingen, Germany from where we were able to reach out to further clients in Africa & Middle East. Partial manufacturing processes began in Germany.

Product Range
In 2002, we expanded our product range to all surgical specialties. Our product range went to 50,000 different types of surgical instruments.

Canada
For the first time we opened up a branch with our own brand in Canada. Now, instead of selling OEM we start to sell with our own brand to dental professionals all over North America.

United States
In November 2023, after much demand from our clients, we opened up our branch in Houston, Texas.

Meet our team

Hassan Tufail

dr. maryyam yousaf

Muhammad Tufail

Waqar Azeem

Aaron Rowe

EDILBERTO VALENCIANO

MUHAMMAD MUTAHAR

ARJUN GUPTA

Nitin Tahilramani

AQEEL HAIDER

HASSAN BHATTI
HITECK VS OTHERS
HITECK
- FREE SHIPPING
We offer Free shipping on all orders, regardless of order value.
- LIFETIME WARRANTY
We offer lifetime warranty against any manufacture, design and material defect.
- CONCIERGE SERVICE
We ship samples to your door free of charge to look at along with a return label.
- 24/7 CUSTOMER SERVICE
We are available 24/7 to assist you on your purchases.
OTHERS
X - NO FREE SHIPPING
There is always a minimum order quantity involved with Free shipping.
X - NO LIFETIME WARRANTY
Very restricted warranty policies. Hard to claim warranty. Have to go through several departments.
X - NO CONCIERGE SERVICE
No other company offers free product samples delivered to your door for evaluation.
X - NO 24/7 CUSTOMER SERVICE
Customer service hours are limited to business hours.
